
Elizabeth suffered from hip pain and needed joint replacement surgery. She was scheduled for surgery and looking forward to a successful procedure that would leave her pain free. On the day of her surgery, she was prepped and ready to go when, after an hour of waiting, her surgeon told her the procedure had been cancelled because it was going to run beyond its scheduled time and into overtime.
Her situation is not unique. Nor is the reason for the cancellation.
Definition of Failure
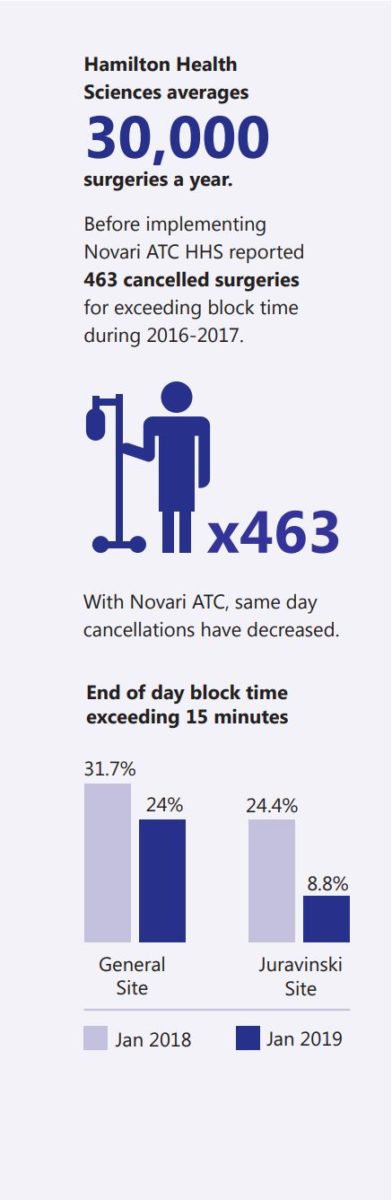
Leslie Gauthier is the Executive Director of Clinical Support Services at the sprawling Hamilton Health Sciences complex (HHS) in Hamilton, Ontario. HHS consists of five hospitals, four of which conduct numerous surgical procedures each day. Three of these are large acute care sites. On an average annual basis, HHS will perform 30,000 surgeries.
Gauthier says a cancelled surgical procedure is her definition of failure. That’s why she spearheaded the effort to onboard Novari Health’s Access to Care (ATC) software module, designed to minimize wait times – and cancelled surgeries – while maximizing available OR resources.
“There’s a lot I can’t control day to day,” she explains, “like if an emergency case bumps in – especially at one of our trauma centres. But I can control if a case is cancelled because the list of surgeries that day is too aggressively booked.” This is an issue that has plagued hospitals for years. The province’s auditor general released a report¹ back in 2009 that detailed recommendations on how to better schedule OR times in order to gain efficiencies and reduce cancelled procedures.
A decade later, the problem is still pervasive across the country.
The Key: Accurate Surgical Bookings
Gauthier maintains that one of the biggest issues at HHS around surgeries lay with far too ambitious case lists compiled by the some surgeons. “If they had a 7-hour block of surgical time, we had a few individuals who would book 9 hours of surgeries. We had the data on average case times and turnaround times that we could show our surgical teams, but it was all a manual process and there were lots of personalities involved in
the discussions.”
Where she needed support was in helping her surgeons accurately book surgeries based on their case lists and the allotted time they had. If they could accomplish this scheduling task, Gauthier knew we would improve our teams finishing work on time. While HHS was incurring extra costs for overtime when surgeries ran late, Leslie Gauthier says money wasn’t the primary issue.
Patients and Staff Come First
“The nurses and anesthesiologists are always the ones who face the pressure of staying late every day. They were getting worn down from a lopsided balance of life perspective with regard to their home life. So, it wasn’t as much about the money as it as about the quality of life for my team.
HHS has had a rule, she says, that a surgery will not be performed if it’s going to run over the blocked time by 15 minutes. Again, there was no universal acceptance of this rule and “lots of grumbling from surgeons.” There was obvious concern for cancelling the last case of the day.
“Hospitals should periodically compare the actual time taken for surgeries—including operating room set-up and cleanup—with the time estimated for completing those surgeries (as indicated by the time booked for the operating room) and identify any recurring significant deviations, so that adjustments can be made to improve operating room utilization.”
— 2009 Auditor-General Report on Management
and Use of Surgical Facilities in Ontario
“There’s a cost to cancellation because time has run out and it’s the patient who suffers,” Gauthier maintains. The average percentage of ORs finishing more than 30 minutes over allotted blocks was around 30% during 2016-2017 – too large a number for HHS. “We recognize that surgeries that run 2 hours over time usually mean something bad has occurred. We can’t control those situations, but we wanted to tackle the instances where surgeries ran 15 minutes to 2 hours over. So, we were trying to solve for the end of the day when cases were running late and to streamline our processes to reduce waste.” When she learned of Novari Health’s award-winning
technology, she knew it was just what HHS needed.
A Visible Tool with Full Transparency
Together with Novari, HHS rolled out the company’s Novari ATC surgical wait list management and eBooking software module in mid 2017. Once a surgeon’s administrative staff learned how to use the technology, the impact became immediately apparent.
“Before Novari, our admin staff in the surgeons’ offices had paper lists of all the patients waiting with their target dates to get surgery. Now, with Novari, they don’t need the paper lists. The surgeon’s office has a complete patient list that comes up on a screen in order of priority with the longest waiting patients at the top of the list. It’s right in front of them. It’s such a visible tool; it’s easy to share and it’s objective. It’s not the piece of paper where who knows if the dates are real? It is real and it’s right in front of people.”
With Novari ATC, surgeon offices schedule their cases within their block according to system generated average case times. Any cases that are required but do not fit within the block forces a conversation with the OR manager to resolve as a team pending available resources. The system indicates the number of times a specific patient was rescheduled and the number of days on the wait list to allow for more informed decision making.
The ATC software automatically flags those patients running out of wait-time. The overall gain for HHS, says Gauthier, is knowing “…which patients, where, and how long they’ve been waiting.”
Gaining New Efficiencies
One of the great strengths of the Novari system – and one recognized by the northwest region which also uses Novari ATC² – is that Leslie Gauthier and her OR manager can see, at a glance, whether or not there is OR time available at other facilities within HHS. “We can then shift some surgical activity to other sites. So, even though my total number of surgical cases hasn’t changed, what has changed is that we have priority 2 cases done in allotted priority 2 times and priority 3 cases done in priority 3 times and so on. We’re able to get way more efficiency out of our system with Novari ATC.”
With any new technology or methodology introduced into a workplace environment, there are the inevitable growing pains and resistance to change. Leslie Gauthier has been very cognizant of that and has rolled out ATC at a gradual pace. “We’ve been very lenient in letting our surgeons get used to the wait time feature [in ATC] and we still haven’t turned on the hard booking tool. We didn’t want to lose our surgeon engagement as we brought the tool online.” The more specific we have built our surgical mnemonics, the more accurate the teams can schedule cases.
The hard booking tool is a feature within the ATC module that prevents a surgery from being booked if it’s going to run over by a set number of minutes, as determined by the hospital, based on historical and accurate physician specific average case times.
Almost a year later, many of our surgeons and their admin staff are starting to tell us, they “just love ATC”, according to Leslie Gauthier. “They love the list, they love being able to book in the pre-op clinic, they love the flags around patients who’ve been pre-oped and are ready to go.”
Cancellations Begin to Drop
HHS reports 463 cancelled surgeries across the three acute care sites during 2016-2017 for exceeding block time, the year before implementing Novari ATC. “That’s 463 patients who had their clothes off, their gowns on, IVs in and they’re waiting to go into the OR when the surgical team agrees to cancel because the room’s overbooked. That’s a lot of people to be sent home.”
That number is already coming down. “The nurses are telling me anecdotally that, at the end of the day, it’s better. And we’re already seeing the blocks that run late trending down, even without the hard booking feature turned on. Once we turn that on, we’ll notice a significant change in the number of surgeries being cancelled.”
So far, the statistics are very encouraging The General Site has seen a reduction in January from 31.7% in 2018, to 24% in 2019; likewise, the Juravinski Site has seen a reduction in January from 24.4% in 2018 to 8.8% in 2019 for the end of day block time, exceeding 15 minutes or greater. “Given that we do 30,000 surgeries across HHS each year, reductions like we’re seeing are tremendously encouraging”, Gauthier states.
A Bright Future with Novari
“I’m happy as hell we went with Novari”, she emphasizes. “It gives us an objective tool to have conversations with surgeons about accurate booking and it’s making the process very transparent. I’m a firm advocate of the Novari system. In fact, we are considering extending it into our diagnostic imaging and interventional radiology areas. It has a lot to offer.”
Novari ATC is having a strong impact at hospitals and in health regions across Ontario and elsewhere in Canada. The software complements and integrates to existing
hospital operating room information systems to include Cerner, Meditech, SIS, PICIS, etc.). Its greatest asset is that it allows hospitals to gain tremendous new efficiencies out of their systems through data gathering and analysis. Not only does a facility and its medical staff benefit but, most importantly, Canadian patients benefit as well.
1 http://www.auditor.on.ca/en/content/annualreports/arreports/en09/409en09.pdf
2 https://www.novarihealth.com/novari-platform-deployed-across-north-west-lhin/