Central Intake and eReferral:
The Solution to Prolonged Wait Times for Mental Health Patients and the Path to Specialist Care

Canadians are not usually described as a smug people; we’re polite, deferential, humble perhaps, but rarely smug. Until it comes to a discussion of Canadian healthcare versus American healthcare. We chuckle at being told our healthcare is “socialist medicine”. Often, we counter with the verifiable fact that no Canadian goes bankrupt because they were ill. In short, when Canadians think about our healthcare system in American terms, yes, we become smug.
The reality is much different. According to the Commonwealth Fund, which ranks healthcare[1] performance among 11 industrialised nations, Canada is third last out of ten nations in overall performance, ahead of France and the United States, which is dead last. Before feeling smug again, consider that our performance suffers when it comes to access to care. Canada sits just ahead of the U.S., in tenth place, second last in other words
Wait Times at Stubbornly High Levels
Access to care is the bane of the Canadian healthcare system; wait times for surgeries have become the stuff of legend over the years and despite endless efforts among the provinces to reduce those times, only mild progress has been made. Despite the billions in spending, despite new hospital construction across the country, despite reorganisation of regional health authorities, particularly in Ontario, nothing seems to have made much of a difference.
When the Covid-19 pandemic shut down all but emergent surgical procedures in Ontario, the impact was immediate; unfortunately, the effect may be long-term. During the initial shutdown period, from March to September 2020, more than 187 thousand previously scheduled elective procedures were put on hold[2] with thousands of new ones not scheduled at all. Hospitals are facing an enormous problem in getting on top of their backlogs.
Mental Health Patients Continue to Suffer
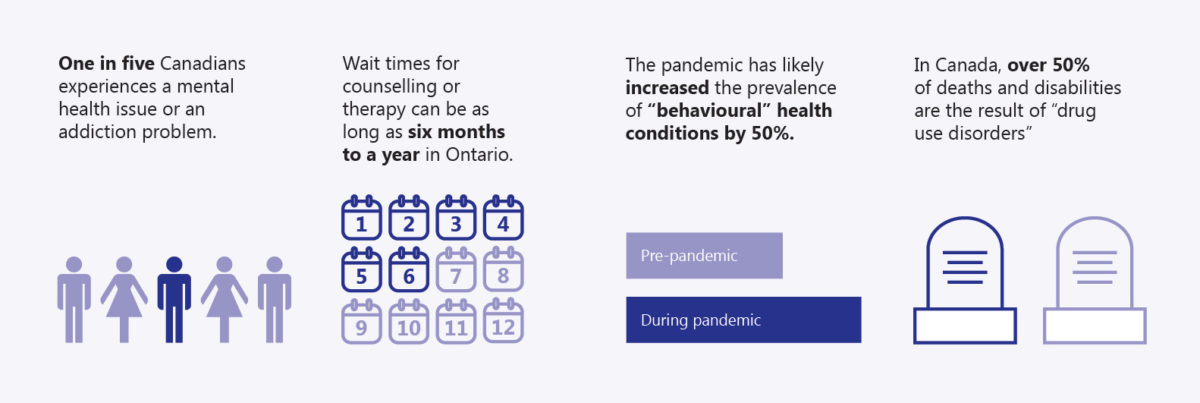
We mustn’t lose sight of the fact that access to care involves far more than surgical procedures. There are many non-surgical health issues that also face unacceptably long and potentially tragic wait times. Mental health is one such problem area. The Centre for Addiction and Mental Health (CAMH) reports[3] that one in five Canadians experiences a mental health or addiction problem. Often, the two go together. To compound this alarming statistic is the fact that, according to CAMH, wait times for counselling or therapy can be as long as six months to a year in Ontario. That may be too long for someone suffering from a psychosis as well as a substance addiction; they may believe that suicide is their only course of action to relieve their suffering.
Other provinces in the country report similar wait times but the evidence is anecdotal. One of the major difficulties in combatting wait times for mental health treatment in Canada lies in the fact that few provinces track them. In the Yukon, for example, the entire system was still paper-based as of 2019 and there were no records being kept, according to an investigative report by Global News[1]. No records are kept at the federal level.
The impact of the Covid-19 pandemic on mental health is as much of a “black swan” event for healthcare as the pandemic itself. According to a report from the think tank, McKinsey Institute, in the United States the pandemic has likely increased the prevalence of “behavioural” health conditions by a whopping 50%.[2] There is no reason to doubt that the same thing has occurred in Canada, as well.
A Smarter Solution
Certainly, more money for healthcare, especially mental healthcare, is necessary. The Institute for Health Metrics and Evaluation reports that, in Canada, over 50% of deaths and disabilities are the result of “drug use disorders”[3]. That is an unacceptably high rate.
But is the wait-time problem one that is solved simply by throwing more money at it? Healthcare spending in Canada has gone from $12 billion in the mid 1970s to more than $264 billion in 2019, according to the Canadian Institute for Health Information.[4] Has it been money well spent? In many cases, yes. However, when it comes to access-to-care, that category where Canada remains second last among industrialised nations, the answer is, unfortunately, no.
An examination of wait times in Ontario, for example, whether for surgical or non-surgical interventions (for example, to treat mental health disorders and others) shows the problem is not simply one of funding. In fact, there are clear, effective and affordable strategies that have proven their usefulness over and over again but still lack full and widespread awareness within the healthcare community and the corridors of power right across the nation.
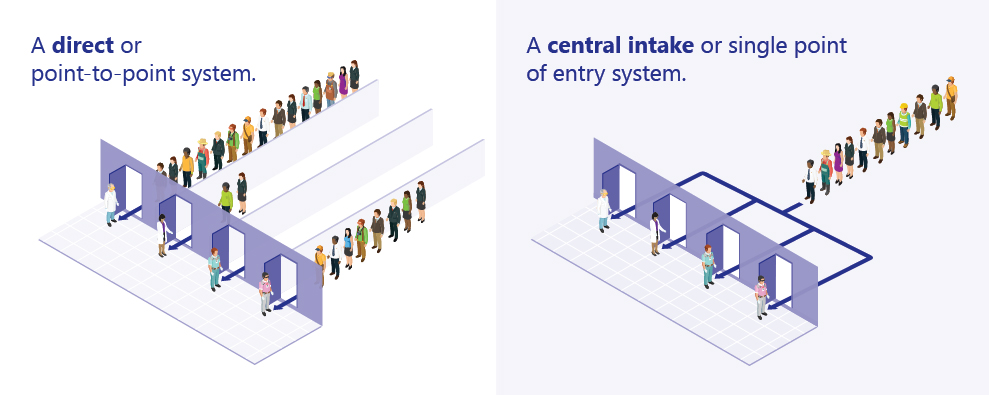
To illustrate the point, consider how shoppers check out at a Walmart store: there is a single entry point into which customers file and wait for the next available cashier. No longer does a shopper fail to pick the right line and get stuck behind someone with a big order. The single intake point funnels customers quickly and efficiently to available cashiers. This same model has been adapted for healthcare use in several regions in Ontario.
One regional that has been using this method, called Central Intake, is the Mississauga-Halton (MH) region. In 2014, the region pioneered what they call one-Link, in order to better identify and refer mental health patients and others (their Central Intake also handles diabetes, foot care and musculoskeletal issues in patients). The system worked well immediately, especially where mental health patients were concerned. Very often, a general practitioner who suspects mental health challenges in a patient will often send a referral to a single psychiatrist to whom the GP has referred patients in the past. When GPs do this on a continual basis, backups occur and wait times become protracted and uneven. Further, it’s commonplace that a psychiatrist is the wrong choice and more time is wasted before the patient gets the proper treatment or counselling. If that same GP submitted a referral through a central intake system like one-Link, patients would be screened by a qualified mental health clinician and then referred to the right provider.
The Next Level for Central Intake
In 2016, the Mississauga-Halton region took another step that supercharged their central intake one-Link programs. They implemented Novari Health’s e-Referral software platform, effectively moving from a paper-based system to a digital, cloud-based system. The effect was immediate, noted Nala Sriharan, the Manager, Coordinated Access, at Halton Healthcare.
“With the regional one-Link program, we have created a single point of contact for clients, families and healthcare providers to access the right addictions and mental health service at the right time. With the Novari eRequest platform, the one-Link program electronically processes high volume referrals with a 150% increase in capacity from a previous paper process. Novari eRequest connects the referring providers, one-Link and receiving services to a single platform and keeps all parties informed with live status updates on every referral. With the Novari enabling technology and coordinated access model, one-Link is able to more quickly connect people to healthcare services.” Sriharan explains. By 2018, the unit had processed over 50 thousand addiction and mental health referrals alone.
When general practitioners fax in their referrals, the Novari e-Referral database records and keeps every incoming fax. No fax is ever lost and no patient’s request for help is ever lost, either. The process is streamlined and fast, so much so that the regional health organisations using Novari’s eRequest technology report reduced processing times of up to 300%. Novari’s referral management and central intake software provides real-time tracking and accurate status reports on patient wait times on every request that it handles. If the Novari system was in use right across the country, wait times would be tracked and accurate reports delivered in every region of every province.
Both time and money are precious commodities in our healthcare system. Too many Canadians are forced to wait for far too long for diagnostic tests or specialist appointments, something that cardiologist and wait time expert, Dr. Chris Simpson, addressed in a recent article in the CMA’s medical journal.[1]
“There are bottlenecks everywhere. A lot of delays are driven by the fact that hospitals operate at very high capacity because there are large numbers of patients requiring alternate levels of care – patients who have nowhere else to go. The interconnectedness of all the sectors in healthcare has been underappreciated, and siloed funding has inhibited the kinds of cross-sector discussions which could improve patient flow. A lot of people still manage waitlists as a stack of paper on the side of their desks, which leads to inefficiency,” he said.
Tearing Down the Silos
A combination of outmoded paper-based systems and inefficiencies in funnelling patients to the right medical providers add up to prolonged wait times. Canada also needs more specialists but, like money, specialists don’t grow on trees, so a better way must be found to handle the backlogs in the current medical system.
GPs are still referring patients to specific specialists because they know no other way to do it. It’s incumbent on the provincial ministries of health across Canada to break down the silos of knowledge that keep awareness of central intake systems hidden from medical providers. How much more smoothly and cost-efficiently could our system run if it were based on the central intake model and powered by a cloud-based technology like Novari eRequest where data is centralised and analysed? Wait time reports are accurate and highlight areas where more attention is needed. The data is available to every member of a medical team regardless of their location and no longer does anyone remain in the dark with no real idea of patient backlogs or wait times.
The need for improved wait times through electronic referral and central intake is widely recognised in the Canadian medical community. The Ontario Medical Association has come closest to pointing to the pressing need for such systems. OntarioMD, a provincially funded subsidiary of the OMA, authored a report in April 2017, pushing for wider adoption of e-Referral systems like that of Novari Health. In recognising the urgent need for adoption of e-Referral systems, the report’s authors state “… patients and physicians are frustrated with the current state in Ontario. Multiple studies over the last several decades have repeatedly identified inefficiencies in referral process. With over 4 million referrals per year in Ontario, quality of care suffers, clinicians are frustrated and health system costs increase.”[1]
The report also points out that the Commonwealth Fund, the organisation that ranked Canada 11th out of 12 countries for access to care, ranked Canada dead last in 2012 for the exchange of electronic information[2]. Seven years later, Canada had moved up just one spot in the same category.[3]
Conclusion
The problem of wait times in Canada is well known, has been well-documented, has received widespread attention in the media and, yet continues to be the biggest hurdle to overcome within our healthcare system. It’s time that Canada stood in the top two in the Commonwealth Fund’s annual rankings, rather than the bottom two year after year.
Referral management and central intake systems like Novari Health’s offer the solution needed to get the country moving in the right direction. In the Mississauga-Halton region, they’ve already seen the benefits for patients, specialists and administrators in reduced wait times, slashed processing time and effort, elevated efficiency and, above all, money saved. If Novari Health’s technology were a publicly traded stock, it would amount to the perfect investment: no risk and healthy returns.
[1] https://www.commonwealthfund.org/chart/2017/health-care-system-performance-scores
[2] https://www.theglobeandmail.com/canada/article-ontario-addresses-two-year-backlog-of-surgeries-hospital-capacity/
[3] https://www.camh.ca/en/driving-change/the-crisis-is-real/mental-health-statistics#:~:text=Costs%20to%20society,health%2Drelated%20quality%20of%20life.
[4] https://globalnews.ca/news/5956330/mental-health-services-access-canada/#:~:text=A%20spokesperson%20provided%20statistics%20for,much%20higher%20at%20112%20days.
[5] https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/mental-health-in-the-workplace-the-coming-revolution?cid=other-eml-dre-mip-mck&hlkid=a774e1a8976d4a078406df70a8406fd5&hctky=11448831&hdpid=fad15aed-40c6-4f4d-8961-88d792c7b476
[6] http://www.healthdata.org/canada
[7] https://www.cihi.ca/en/national-health-expenditure-trends-1975-to-2019
[8] http://cmajnews.com/2020/08/28/access-qa-1095895/
[9] https://www.ontariomd.ca/documents/lhin%20reports/ontariomd%20-%20provincial%20ereferral%20initiative%20business%20case%20v0.7.pdf
[10] The Commonwealth Fund – A Survey of Primary Care Doctors in Ten Countries Shows Progress in Use of Health Information Technology, Less in Other Areas, 2012
[11] https://www.commonwealthfund.org/publications/surveys/2019/dec/2019-commonwealth-fund-international-health-policy-survey-primary